Have you ever felt like you are on an emotional roller coaster when you see your blood glucose (sugar) readings going up and down with no clear explanation? Have you experienced times when no matter what you do, you cannot seem to get off the roller coaster? If the answer is yes, please be assured that you are not alone!
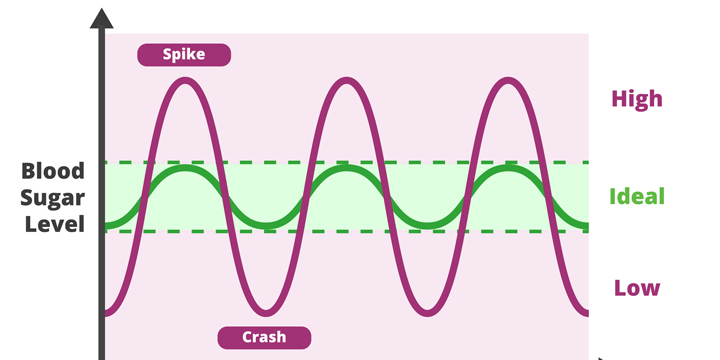
Variability in blood sugar is a continuing source of annoyance for people with diabetes, sometimes driving them to stop checking it. However, blood sugar variability can lead to many complications. So, before you admit defeat, let’s investigate how you can deal with this frustration in a more positive way.
The first step is to understand why there is variability in your blood sugar values. With this knowledge you can better reflect on what factors can affect your readings. The second step is setting realistic goals. The third step involves investigating more helpful self-talk. Since frustration is a self-generated response, you need to practice self-compassion.
What affects blood sugar?
You have likely been taught that the food you eat, the activity you engage in and the medications you take can all affect your blood sugar. These are the obvious culprits, but have you considered other factors, such as pain, dehydration, altitude, anxiety, hormonal changes, sleep habits and stress? As Adam Brown states in his book “Bright Spots and Landmines,” there are at least 42 factors that can affect your blood sugar. The suggestion is that you need to be your own detective. Take some time to accurately record your food intake, activities and emotions, as well as your blood sugar readings. Repeat these recordings on different days of the week. Do you notice any patterns? Are there any particular foods or certain activities that affect your blood sugar, either in a positive or negative direction? What does stress do to your readings? Are your levels improved with a good night’s sleep? Awareness is knowledge that you can work with.
To help explain blood sugar excursions, it’s a good idea to familiarize yourself with some of the excellent tools available. Understanding food labels and mastering the handy portion guide for portion control are beneficial techniques for deciphering information about food and portion sizes.Bottom of Form There are so many additives to foods that may be affecting your blood sugars. Also keep in mind that aerobic exercise versus resistance exercise can have different effects on your blood sugar. The current technology for measuring physical activity can provide a wealth of information to help us interpret our blood sugar levels.
Setting realistic targets
Armed with the knowledge you now have as to what affects your blood sugar, your next questions are: “What target values are realistic for me to work towards?” “How much blood sugar variability is okay, and when should I be concerned?”
Regardless of the method you are using to measure your blood sugar, the targets for most people with diabetes are 4 to 7 mmol/L before meals and 5 to 10 mmol/L 2 hours after meals (or 5 to 8 mmol/L if your A1C target is not being met). These values equate to an A1C of 7% and a >70% time in range.
If you are using intermittent or continuous glucose monitoring systems, your downloads will have a measurement of the % of time in range, % of glycemic variability and standard deviation. Speak with your diabetes healthcare team about your appropriate targets.
Since diabetes is a very personal condition, all of your blood sugar targets need to be individualized to your life and your needs. Age, medications (especially steroid use) and comorbid conditions such as heart failure or kidney disease, will all factor into your and your healthcare team’s decision regarding the best target range for you to aim for.
Once you have set up a realistic target range for your blood sugar levels you need to work with your expectations. Your goal here is to manage your blood sugar, not strive for perfection. Even people without diabetes see fluctuations in their blood sugar. You too will see these fluctuations despite your best efforts. Many people with diabetes see this as a failure. Feelings of guilt and self blame may surface, creating endless frustration. You deal with this by realizing that you can control some things, but many other factors are outside of your control. That’s why it’s important to engage in the act of self-compassion.
Engaging in self-compassion
In simple terms, self-compassion is the ability to be kind to ourselves. Kristin Neff, a psychologist known for pioneering research on self-compassion, has suggested that there are 3 components to self-compassion: self-kindness versus judgment, common humanity versus isolation and mindfulness versus over-identification.
Applying this principle directly to your frustration with ‘imperfect’ blood sugar readings, you need to initially stop judging yourself by the numbers you see. By gearing your self-talk to the positive aspect rather than centering on the negative, you aim to see the trend to improvement. Rather than dwelling on the high number, you can look at the trend, and use your investigative skills to continue in the positive direction.
You also need to remember that you live in the real world. Your human instincts direct you towards pleasure, and you will occasionally eat that chocolate bar or that fabulous piece of chocolate cake. This is not failure but simply being human. One high reading does not alter your A1C nor dramatically change your time in range. Allow yourself to deal with your diabetes in the context of real life.
By living in the present and recognizing that your blood sugar readings do not define you, it is easier to develop a healthier mindset. By engaging in positive self-talk and self-encouragement with more realistic goals, you can decrease the frustration you have previously felt. Utilize your expertise and abilities in diabetes care to continually pursue enhancement, while acknowledging that perfection is an unattainable standard for any individual.
You can take yourself off the roller coaster!