In Canada, 8% of the population lives with type 2 diabetes and 285,000 people live with type 1 diabetes. These numbers will continue to grow because the number of people diagnosed each year is increasing for both type 1 and type 2 diabetes. Fortunately, medical advances have led to people with diabetes living longer and healthier lives. This article highlights some of the recent advances and current trends in diabetes management in Canada.
Weekly insulin
In the summer of 2024, Canada became the first country to launch the world’s first weekly insulin. Insulin icodec (Awiqli®) is injected similarly to other insulin pens but can be given just once per week due to its unique formulation. Insulin icodec provides similar benefits for blood sugar levels as daily insulin, but offers greater convenience for people living with diabetes. Insulin icodec can be used by people who are just starting an insulin regimen or as an alternative for people who are already using daily insulin.
New weight loss medication options
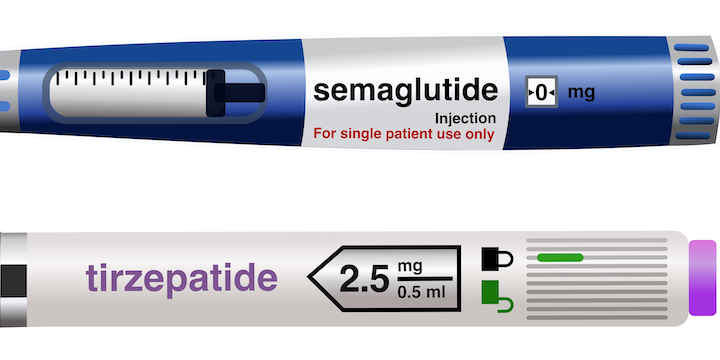
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medication indicated for diabetes and weight loss that have been very popular and have received a lot of attention in the media. These medications are administered weekly and include semaglutide (Ozempic® and Wegovy®). Tirzepatide (Mounjaro®) is a related medication; it is a GIP (glucose-dependent insulinotropic polypeptide)/GLP-1 agonist, and has also been found to be very effective for weight loss.
These medications are used in people with type 2 diabetes, particularly if they also have heart disease and/or high blood sugar levels despite using other diabetes medications. Currently, Wegovy is the only weekly GLP-1 receptor agonist available in Canada for weight loss in people who do not have diabetes.
Prioritizing heart and kidney health
Diabetes management is evolving from being ‘glucose-focused’ to being ‘organ-focused.’ Although regulating blood glucose levels is still important, diabetes healthcare providers are now prioritizing glucose-lowering medications that also have benefits for the heart and the kidneys. This is even more important for people who already have heart or kidney disease, or risk factors for developing these conditions. Both sodium-glucose cotransporter 2 (SGLT2) inhibitors and GLP-1 receptor agonists prevent heart attack, stroke, kidney impairment and death, and are commonly used for people with type 2 diabetes.
Continuous glucose monitors
Continuous glucose monitors (CGMs) are small devices worn under the skin that measure glucose levels every few minutes. This data is sent to a handheld device or smartphone, allowing people with diabetes to track their glucose in real time. These devices can also alert users when blood sugar is too high or too low. While costs have decreased, CGMs remain out of reach for many due to limited public program coverage.
CGMs are especially common among people using insulin, and are even expanding to those not on insulin. For individuals using CGMs, diabetes healthcare teams may focus on ‘time in range’ (the percentage of time glucose levels stay between 3.9 and 10 mmol/L) rather than just A1C.
Virtual care
Since the COVID-19 pandemic, virtual healthcare has become more common. Diabetes management appointments by video or phone are now a frequent option, especially for reviewing blood sugar levels, which can be shared via cloud or download. However, many healthcare providers still prefer to see patients in person at least once a year for essential checks, such as blood pressure assessments and foot exams.
Expanding access
While the developments in diabetes medications and technology are exciting, ensuring access for everyone who could benefit is critical. Public funding for newer diabetes treatments and CGM has expanded in some provinces, but gaps remain. A proposed national pharmacare program, which is making its way through the legislature, could help ensure that all people with diabetes have access to the medications and devices they need.